

Today we’d like to introduce you to Kelly Mccall.
Hi Kelly, thanks for joining us today. We’d love for you to start by introducing yourself.
I’ve always been drawn to deeply intimate, service-oriented work. At 58, I look back and realize that guiding people through their most vulnerable moments wasn’t something I chose—it chose me. My path led me naturally to becoming a death doula, where every conversation, touch, and silent vigil holds profound meaning.
I began in hospice care, elder care, and supporting family members death & dementia. Those experiences taught me how grief reshapes our world and how vital it is to hold space for both the person who’s dying and their loved ones. There’s so much fear and uncertainty in that journey, and stepping in as a steady presence became my calling.
To refine my practice, I trained with Maui’s Doorway Into Light and earned certification through INELDA. My approach blends hands-on care, massage therapy (I’ve trained in Swedish, Northern Thai, and sports techniques), and a deep well of knowledge on end-of-life options. Whether it’s deciding when to start hospice care, exploring home funerals, navigating assisted living, or offering emotional and spiritual support—I guide people gently and pragmatically.
My role often feels like that of a bridge: between medical staff and family caregivers, between life’s final chapter and the legacy we leave behind. Along the way, I’ve been a hospice volunteer and nurtured a massage practice that soothed bodies and hearts alike.
At its core, my work is about presence—being there, without agenda, for the raw, tender moments. I listen to every question, honor every emotion, and create space for dignity and connection. Whether it’s a late-night vigil or a quiet ritual at dawn, I walk beside people when it matters most.
So, how did I get here? It started with a life of showing up—then learning how to show up better—and finally, realizing that helping people face death with compassion is not just work. It’s my purpose.
Can you talk to us a bit about the challenges and lessons you’ve learned along the way. Looking back would you say it’s been easy or smooth in retrospect?
Becoming a death doula hasn’t been a straight shot — it’s been a tightrope. Here are the biggest challenges I’ve faced:
• Emotional weight – Holding space for grief, over and over, will test your limits. I needed therapy, time in nature, and boundary-setting like a reflex.
• No roadmap – This field is still carving itself out. I cobbled together trainings, mentors, and best practices one piece at a time.
• Death stigma – Even “death-positive” people squirm. I’ve learned to listen first, share later, and never push.
• Training costs – Courses aren’t cheap. I juggled side gigs and crowdfunding just to stay certified.
• Defining my role – I’m not a medical provider or lawyer — I’m the emotional and ritual guide. It took time to draw that line clearly.
• Gaining trust – At first, I felt like a fraud. But showing up, again and again — being quietly reliable — that’s what built connection.
Every awkward conversation and messy farewell has reminded me: this work is hard, but it matters.
Thanks – so what else should our readers know about your work and what you’re currently focused on?
At the heart of my work is a deep belief in the power of elders, village-making, and community. It was and is guidance from wise teachers like Stephen Jenkinson that help me understand and remember this calling isn’t about fixing death—it’s about being with it, honoring the dance of grief, presence, and ritual. That kind of learning happens in circles, not classrooms—through listening, reflection, and unspoken strength.
As I do my best to stay on this path, I am constently reminded that true elderhood isn’t about stepping back—it’s about being visible, bringing others into the circle. So I mentor new doulas—not just in practical skills, but in building their inner resilience, compassion, and sense of belonging. I hope we can stitch together a village of care—so no one faces life’s most vulnerable moments alone.
In terms of your work and the industry, what are some of the changes you are expecting to see over the next five to ten years?
⸻
🌱 1. Professionalization & Credentialing
What began as grassroots support is now becoming standardized. Membership in the National End‑of‑Life Doula Alliance jumped from around 260 in 2019 to over 1,500 in 2024, and structured training programs are increasing. Expect to see formal certifications, ethical codes, and even state-by-state licensing emerging .
⸻
🤝 2. Integration with Healthcare Systems
Hospice and palliative care programs are beginning to treat doulas as valuable members of care teams—offering emotional, spiritual, and logistical support. Health systems are exploring pilot programs that embed doulas in end-of-life care . It’s becoming standard to pair medical care with compassionate doula services.
⸻
🎗️ 3. Cultural Acceptance & Innovation
The “death-positive” movement and post-pandemic awareness have opened up conversations about mortality. This cultural shift, combined with a rise in personalized funerals, green burials, and legacy rituals, is creating fertile ground for doula-led services .
⸻
📑 4. From Legal Gray Zone to Recognized Profession
Currently, the field operates largely without regulation—but change is coming. With Medicaid now covering birth doulas in some states, death doula advocates are pushing for similar recognition. In Georgia, for instance, pilot programs are exploring doula reimbursement, and discussions are underway about insurance support for advance care planning and voluntary stopping of eating and drinking (VSED) accompaniment .
⸻
🌍 5. Adopting the “Midwife Model” for Death
The end-of-life midwife model is growing—supporting families through home funerals, ritual planning, and after-death care. Much like birth midwifery, this holistic approach is resonating with communities seeking deeper cultural and personal meaning in how they say goodbye .
⸻
In summary:
Death doulas and midwives are on the brink of a major shift—from compassionate sidelines to essential components of end-of-life care. As standards are formalized, healthcare systems embrace them, and society becomes more death-literate, their work isn’t just filling a gap—it’s reshaping how we approach the end of life.
— Kelly McCall
Pricing:
- Tier 1 | $0-$75 per hour
- Tier 2 | $75-$125 per
Contact Info:
- Website: https://www.colorpool.org



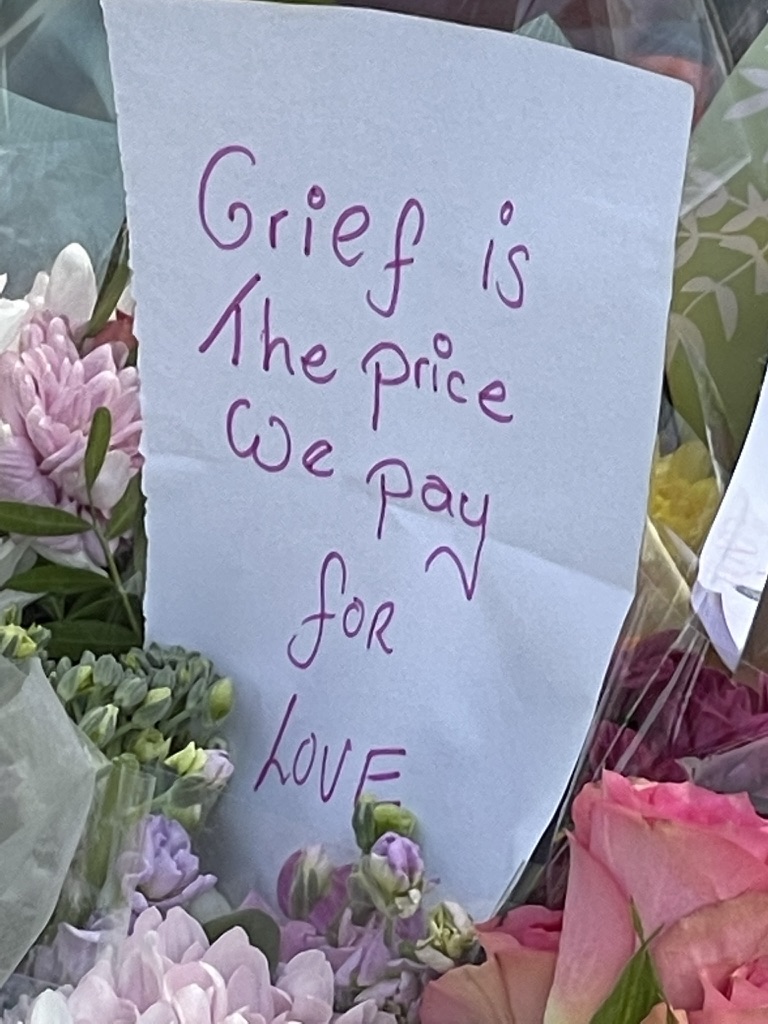
Image Credits
They are all photo’s I have taken. Me with a client who took Medical Aid In Dying meds because she had a terminal illness. A memorial at the beach. A client who had just died who we bathed and adorned at home. A note at a memorial.














